Abstract
Sickle cell disease (SCD) is a severe hemoglobinopathy due to abnormal hemoglobin S (HbS). One of the most serious complications of SCD is cerebral vasculopathy (CV) leading to ischemic stroke in 8% of homozygous SS children without prevention strategy. Typical CV in SCD is a stenosis of one or more intracranial or cervical arteries, including internal carotid arteries, anterior cerebral arteries and middle cerebral arteries. However, several studies have reported the occurrence of stroke in SCD children in the absence of typical cerebral vasculopathy.
The aim of the study is to investigate the prevalence of stroke without CV in SCD children, and to compare them to "classical" stroke (i.e in a context of typical CV) in terms of suspected etiologies, triggering events, treatment and risk of recurrence.
In a large cohort of about 1500 SCD children living in Paris area, France, we recorded all the strokes occurring between 2007 and 2020, excluding venous thrombosis and PRESS Syndrome. These children were followed in a university hospital, and all benefited from early screening for cerebral vasculopathy and an adapted stroke prevention program. We considered as a "typical" stroke any new ischemic lesion of the cerebral parenchyma associated with an acute neurological syndrome occurring in the territory of a pre-existing and/or non-regressive stenosis.
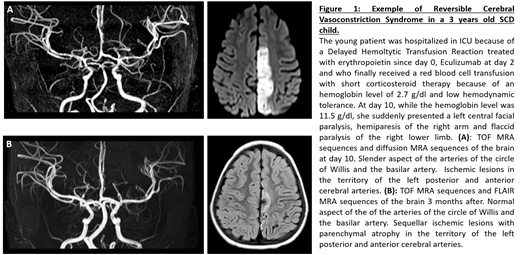
25 strokes occurred during the study period. 12 of them (48%) did not met the definition of a "typical" stroke related to sickle cell CV. The children with "atypical" stroke were older (9 years old +/- 4.6, vs 6.5 years old +/- 4.3 in the typical group, p = 0.0086) and less frequently of SS genotype (33% non-SS vs 8% non-SS in the typical group). They had lower leukocyte count (11.3 G/L +/- 4.6, vs 15.7 G/L +/- 2.3 in the typical group, p=0. 04) and higher hemoglobin level at the time of the stroke (11 g/dl +/- 3 vs 7.4 g/dl +/- 1.3 in the typical group, p= 0.027). 17% of atypical strokes had posterior ischemic lesions, 33% had anterior lesions and 17% had multiple systematized lesions, in counting junctional lesions. We also found 33% of ischemic lesions of the cerebellum. Considering a potential trigger of the stroke, 58% of atypical events were hospitalized in an anesthesia or intensive care unit at the time of the stroke or less than 7 days before, compared to 8% of children with a "classic" stroke (p= 0.011). The etiologies adopted by clinicians and radiologists for the atypical stroke were reversible cerebral vasoconstriction syndrome (RCVS) (Figure 1), cerebral fat embolism, hyperviscosity and vasculitis in systemic inflammatory context. The evolution in the atypical group was more favorable in terms of recurrence (0% within 2 years vs 42 % in the typical group, p= 0.045), although only 33% (3 children) of atypical strokes were still under exchange transfusion program 24 months after the stroke vs 92% in the group of typical stroke.
Overall, in a cohort of SCD children with efficient stroke prevention program, atypical strokes account for nearly half of all acute ischemic neurological events, related to hyperviscosity, RVCS or inflammatory vasculitis. Physicians must be aware of the potential triggers and of the context in which such events occur. Nevertheless, stroke without CV may not require long-term transfusion program contrary to stroke with CV, given the very low risk of recurrence we highlighted.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal